Ethical Surrogacy Blog Series
Starting out — knowing if you are ready
Ethical surrogacy in Australia and overseas — are you ready
A deeply personal and practical guide to deciding if you’re ready for ethical surrogacy, grounded in lived experience across Australia, Canada and Argentina.
Surrogacy is not a neat checklist. It is a long road where science, law and love intersect — and sometimes collide. If you’re at the beginning, the most honest question is not “Can I afford it?” or “Which country?” It is “Am I truly ready for what this will ask of me?”
I didn’t start with spreadsheets. I started with a jolt. At thirty‑two, during a musical theatre contract, my heart stopped. I was placed in a coma and later diagnosed with Brugada Syndrome. Doctors told me survival had been around five percent. Waking up to that number reordered my life in a single breath. Family moved from ‘someday’ to ‘now’. My partner and I decided to do more than talk. We would act.
Readiness is not perfection — it’s acceptance
Readiness looks like accepting three truths:
You will lose control many times. Doctors, coordinators and the woman carrying your child will make decisions with you and sometimes for you.
There will be setbacks. Even when you do everything right.
You will be asked to trust — again and again — and to keep showing up with kindness.
Emotional readiness
You are not purchasing a service; you are forming a relationship that becomes part of your child’s origin story. Are you comfortable building a friendship with your surrogate, sharing updates, agreeing boundaries, and staying present through scans and silence alike. Counselling helped me sit with the mix of hope and grief that coexists at the start, especially after loss.
Practical readiness
Australia’s system is altruistic. There are no matching agencies. Most people meet in community groups and invest months building trust before any medical step. That can be beautiful; it can also be slow and uncertain. Ask yourself: can you make time for counselling, medical screening and legal work. Can your life absorb extended overseas travel if you go abroad. Do you have a support plan for older kids at home.
Ethical readiness
Commit to principles you won’t bend: informed consent for everyone, independent legal advice, genuine psychosocial support for the surrogate, transparent fees and communication, and a relationship that treats her as a person, not a process. If any program discourages contact with the surrogate, walk away.
My first hard lessons
We did a surrogacy journey in Australia. We met generous women, did the counselling and legal work, and created a single embryo with a family egg donor. We had a positive test. The numbers didn’t double. We lost that pregnancy at an early stage. People who haven’t sat in fertility clinics sometimes say “it wasn’t really a baby.” It was hope made visible — and then gone. It hurts.
Before that, we had tried Thailand. The offers were plentiful and the red flags were everywhere — though I didn’t have the vocabulary yet. Poor embryo quality. Advice pushing multiple transfers. The clinic even did a triple‑embryo transfer, we’d never agreed to this but we were told “none are likely to take.” Looking back, I shudder. It’s now very rare that any surrogacy would have any more than one embryo transferred.
Then the country shut its doors: a military coup, a clinic closed, a doctor arrested. Overnight the program collapsed during the Baby Gammy era. It was traumatic for intended parents and surrogates. I learned the first non‑negotiable of readiness: if you feel rushed or discouraged from asking questions, leave.
What readiness looks like in practice:
• Set an update rhythm with your surrogate or coordinator (we used WhatsApp).
• Plan buffers: babies don’t read calendars; in Argentina,I missed my daughter’s birth when she arrived four weeks early.
• Organise documents in one digital folder with dated notes.
• Build community: peers who understand will keep you steady between appointments.
• Budget honestly with space for longer stays, translations, and flights that change twice.
The heart of it
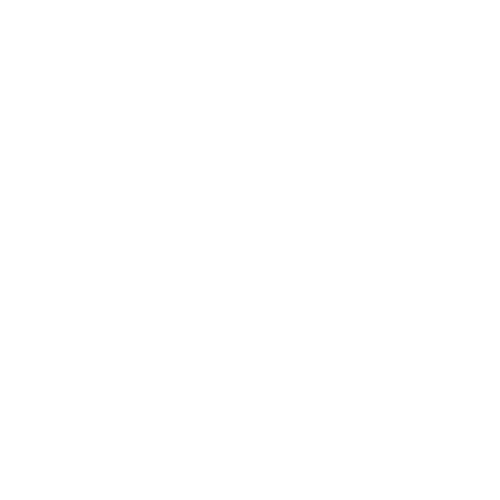
After a near‑death experience, I found life in unexpected places: a son born in Canada, a daughter in Argentina, and friendships that stretch across continents. Readiness wasn’t a perfect plan. It was saying yes with open eyes and staying kind when the road bent.

Starting out — knowing if you are ready

Domestic surrogacy or overseas — how I decided (with every messy detail)
Selecting an agency or program — every question I wish I’d asked

Choosing a country if going overseas — deep dive, no gloss
Domestic surrogacy or overseas — how I decided (with every messy detail)
Domestic vs overseas surrogacy — an Australian’s real decision
Australia’s altruistic pathway, a collapse in Thailand, failures at home, Canada’s structure and Argentina’s fit. Every step I took and why I changed course.
Choosing between Australia and overseas is not academic for me — it is lived, with scars and joy.
Australia first: friendships, counselling, law — and no baby
Australia’s strength for local Intended Parents like me is that the distance, and often language, is not a barrier. There are no agencies or matching services. You meet in Facebook groups and community spaces, you visit each other’s homes, you do counselling and independent legal advice. That process gave me some of my closest friendships. It also gave me two crushing early losses — including one where the positive test became a call while I was on a bus about bleeding and falling HCG.
This journey ended in a traumatic early labour and miscarriage at home. Two families held each other up. That is the truth of domestic surrogacy: beautiful intent, heavy time cost, uncertain outcomes. What’s not so good is the waiting to be matched, there’s a very clear ratio imbalance between surrogates and Intended Parents. It often takes years to build trust before an offer is made and unfortunately, sometimes without proper screening on both parties, matches are often misguided.
Thailand: the chapter I wish I could rewrite
We started looking offshore around 2012. Conferences, glossy promises, and an idea to use a split cycle so two surrogates could carry at once — half embryos created with my sperm, half with my then partner’s.
We flew in a donor from South Africa; there were no mature eggs. We tried again with a donor from Poland; embryo quality was poor.
We were advised to transfer three embryos at once because “it probably won’t work.” Imagine if all three had implanted, or one had split.
Then came the Baby Gammy scandal, along with some other surrogacy scandals in Thailand, a military coup, clinics closed, a doctor arrested, and foreign surrogacy effectively banned.
We found out on the day of a failed transfer. Trauma layered on trauma — and I had further cardiac episodes under the stress. Lesson learned: red flags ignored become disasters you have to live through.
After the whole saga left us emotionally and financially ruined, my sister offered to donate eggs. We found a local surrogate in Australia and began the process of getting to know her. We became great friends and eventually she offered to be our surrogate mum. We were over the moon. We did the counselling, legals, my sister donated eggs and we had one beautiful little embryo, ready to transfer.
The transfer took! She was pregnant. We thought we had everything in life we’d ever asked for. My then partner even booked the embryo into daycare because ‘you have to get in early for a good spot!’.
Unfortunately it wasn’t to be and the pregnancy was lost pretty early.
It was devastating for everyone involved, particularly because we only had the one embryo.
Canada: structure with heart
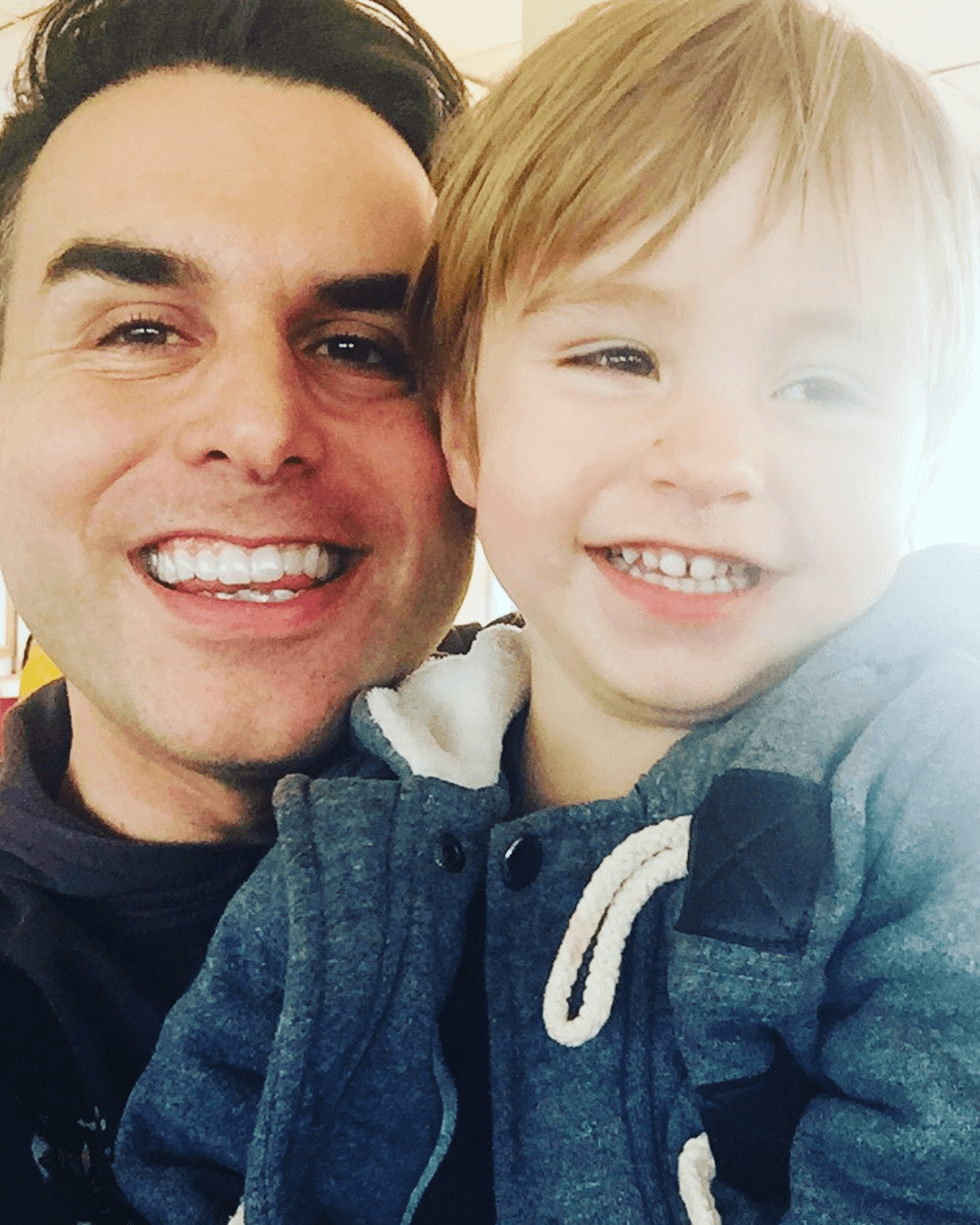
A Facebook group introduced us to a woman who had carried a set of twins before and had four children of her own. Her IVF doctor called her uterus “a Cadillac”. We created embryos via a Canadian donor (split cycle again), did one transfer and it worked first go.
Even though we were speaking five times a day, we only met our surrogate in person at five months when we went to see her and her family in Canada.
The journey was smooth, Orlando came along, we went over and had six beautiful weeks with him, our surrogate and her family. My mum came over to help for the last few weeks too.
We Orlando home after six weeks in Ontario — we stayed in Stratford, the town famous for the Shakespeare festival fame and yes, Justin Bieber’s hometown.
Orlando’s surrogate even pumped enough milk that we flew home with frozen bags to give Orlando a little each day for six months.
Canada showed me what respectful structure looks like: screening, consent, independent legal advice, and warm, frequent communication.
Life still happened. My partner and I separated when Orlando was eight months old. We briefly reconciled and separated again. The relationship with our surrogate remained strong — a reminder that surrogacy relationships can outlast romantic ones and become family in their own right.
Trying again in Australia: hope, then heartbreak (twice)
I wanted Orlando to have a sibling. We matched locally quite quickly with a beautiful woman and her family. We became close very quickly.
We did legals and counselling. One embryo from Canada was shipped over. A positive test. Then the call: bleeding, bad numbers. We flew to Adelaide anyway to be together — kids in the back seat, a beach trip that became triage at home. She was in the small percentage who go into labour even at a very early stage.
Afterwards she said she was willing to try again — even as a traditional surrogate via at‑home insemination (“turkey baster” and all). We made plans. Ultimately, time and life made that path unsustainable. I was in my mid‑forties; Orlando was starting school. I could not spend years courting luck again.
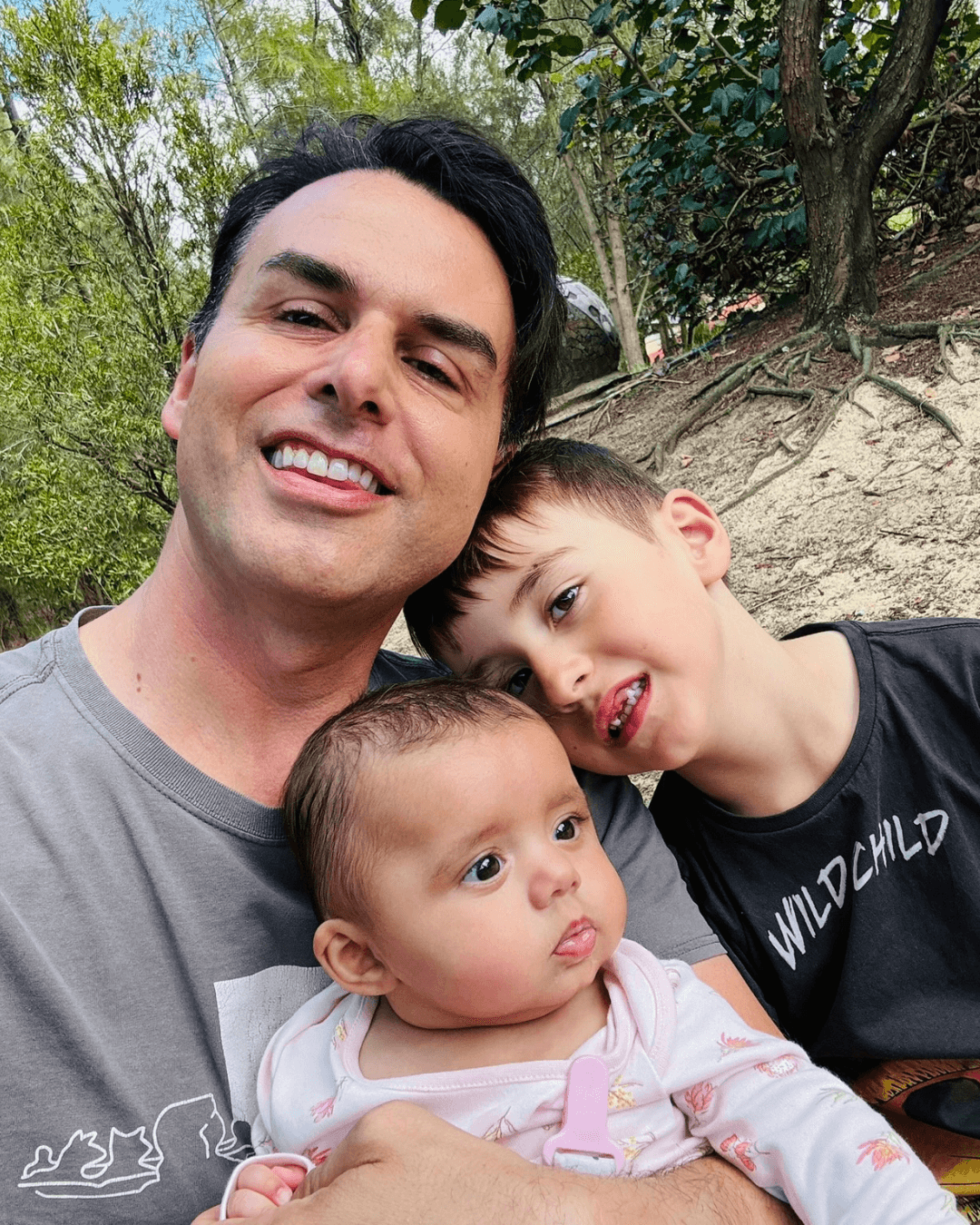
Argentina: the fit I didn’t expect
The US was beyond my budget. Canada now had long waits. I consulted on Mexico and Colombia. Then I looked at Argentina. I’d always wanted to go there, the beautiful cities, great food and culture and beautiful people. I quite quickly fell in love with the idea and signed up and went over.
Now that I’m working in surrogacy, I always tell many potential clients to not do what I did, even though it worked out so well for me. From the moment I had the first consult to the moment I signed up, was two weeks. I was done at that point and just wanted to get the wheels in motion.
We generally say to talk to as many agencies as possible and take a month or two to decide. I didn’t, I had the feeling straight away that the agency I chose and the destination, at the time, was the smoothest possible outcome for our family.
I flew over, did the consultations and did the sperm deposits. Argentina was exactly how I imagined it. I loved it from the very beginning.
I didn’t speak Spanish and my future surrogate didn’t speak English, but the cultural fit — strong psychotherapy culture, solid medical training, and a legal pathway that puts intended parents on the birth certificate — mattered.
In Buenos Aires, I reviewed about 35 donor profiles, matched with a beautiful donor with a very kind face and one who the donor coordinator said matched what I was looking for. Someone kind, funny and creative.
The clinic created embryos: 18 mature eggs, all fertilised; 12 day‑5 blastocysts. Because there were many embryos I chose PGT‑A.
The first transfer worked.
The language barrier became a bridge. We texted through a translator. She asked for playlists to play to “our girl”. I asked not to be told embryo sex; a well‑meaning doctor rang me directly and blurted, “We’re putting in the girl.” I laughed and cried and told my mum, who had already been campaigning for a granddaughter.
Frida arrived four weeks early while I was at the hardware store buying a toilet seat for a last‑minute Airbnb renovation to fund the stay. I missed the birth by four and a half days after a 36‑hour set of flights with no direct options left. Those first cuddles were still perfect. We stayed just over three months because paperwork on the Australian side took longer than average (timelines are faster now, though they can still vary).
Somewhere in the first four weeks, wearing my baby in a carrier, I met my partner. Not a conventional way to meet your other half, but it worked for us.
Later my mum and Orlando joined, and between appointments we even took a short trip to Mendoza with coordinators who had become friends.
How to choose your path (questions I now insist on)
• Ethics first: Do they welcome surrogate‑parent contact. Is independent legal advice standard for all parties. Is counselling ongoing.
• Clarity over speed: Who updates you and when. What exactly happens after a failed transfer. What’s the plan if the baby arrives early.
• Legal map: Birth certificate steps, translations, typical stay length, and what happens if an office interprets a rule differently this month.
• Budget reality: Flights, long stays, translators, insurance, visas. Build a buffer you don’t touch unless you must.
• Gut check: If you feel rushed, patronised or kept at arm’s length from your surrogate, it’s a no.
The answer
There is no universal right choice. Australia gave me friends for life. Canada gave me my son and a surrogate who is a part of our family. Argentina gave me my daughter, again a surrogate mum who is part of our family — and a bigger family than I knew to wish for. Your right answer will look like the place where your values, budget and temperament overlap.

Starting out — knowing if you are ready

Domestic surrogacy or overseas — how I decided (with every messy detail)
Selecting an agency or program — every question I wish I’d asked

Choosing a country if going overseas — deep dive, no gloss
Selecting an agency or program — every question I wish I’d asked
Choose an ethical surrogacy program — the definitive checklist
From screening and counselling to updates, fees and early‑birth plans, here are the specific questions and red flags I use after Canada and Argentina — with no provider names.
When choosing a clinic, what matters is the detail in writing and how a program behaves under stress. These are the exact questions I now ask — and why.
1) Where do you operate — and why not elsewhere
Responsible programs can explain their jurisdiction choices in plain language: workable law, clear parentage pathway, hospital cooperation, translator availability, and a culture of consent. If the answer is “because it’s cheap” or “because we can,” keep walking.
2) Screening, counselling and social safety
Ask for specifics: medical criteria for surrogates, psychological screening tools, frequency of counselling (Argentina’s culture of psychotherapy was a genuine plus), and social checks — including support networks and domestic safety. You want a surrogate who is well, willing and well‑supported.
3) Independent legal advice for everyone
Non‑negotiable. The surrogate must have her own lawyer. So must you. Contracts should cover contact expectations, decision‑making, expenses, insurance, early‑birth scenarios and post‑birth contact — in language everyone understands.
4) Communication — cadence and channels
Who updates you after bloods, scans and OB visits. How quickly. Is there a WhatsApp group with the coordinator, surrogate and you, or a structured portal. Agree the rhythm up front. Anxiety thrives in silence.
5) Early births and hospital plans
Babies arrive when they like. Ask what happens if you’re not yet in country. Who is allowed in the room. What are the hospital’s ID rules for skin‑to‑skin and discharge. Who translates at 3am. Where are documents stored and who brings them.
6) Fees — inclusions, exclusions and timing
Request a line‑by‑line schedule. What is covered (screening, transfers, meds, legal, counselling, translations, pregnancy care) and what is not (NICU, extra scans, embryo testing, additional legal steps). When are payments due and what triggers them.
7) Law and policy changes
What is the formal plan if a registry slows birth certificates or an office interprets a step differently this quarter. Who escalates. What support does the surrogate receive if the stay extends. Ask for a written protocol.
8) References
Speak to recent parents (last 6–12 months) in your language and from your country. Ask them what went right and what went wrong and how it was managed. A good programme welcomes this.
Red flags I’ve lived
• Being told to limit contact with the surrogate “to avoid awkwardness.” Never accept this. If you’re told this, someone is getting ripped off, either you, her, or possibly both of you.
• Vague answers about legal steps like getting on the birth certificate.
• Pressure to move fast or transfer multiple embryos “just in case.”
• Resistance to sharing draft contracts or to your surrogate obtaining independent advice.
• No documented plan for early birth or administrative delay.
What good looked like for us
Canada: consent, clarity and respect, with a lot of self‑navigation. Argentina: structured coordination, ongoing counselling, and a relationship‑friendly approach, with the trade‑off of language and some variable admin timelines. In both places, the people made the difference — coordinators who answered questions, doctors who listened, and surrogates who became family.
Final word
Do not be dazzled by brochures. Be guided by detail and how you can relate and communicate effectively with those who’ll be guiding you on the journey. People who welcome your questions now will stand beside you when the road bends later.

Starting out — knowing if you are ready

Domestic surrogacy or overseas — how I decided (with every messy detail)
Selecting an agency or program — every question I wish I’d asked

Choosing a country if going overseas — deep dive, no gloss
Choosing a country if going overseas — deep dive, no gloss
Overseas surrogacy for Australians — country‑by‑country deep dive
A values‑led, practical, and candid analysis of the main destinations for international surrogacy in 2025. Pros, cons, timelines, red flags, and who each option suits. Colombia and Mexico treated separately. Georgia included.
Laws and policies change. Treat this as orientation, not legal advice. Always obtain current advice from lawyers in Australia and in the destination country.
Canada (altruistic, but regulated by agencies, strong structure)
What works: Clear consent framework, independent legal advice standard, relationship‑friendly culture, English‑speaking, robust clinic network.
Trade‑offs: Matching can take years, you will need to sell yourself as an Intended Parent as the surrogates obviously have a lot more choices; you’ll self‑coordinate more than in concierge‑style programs; costs higher than Latin America; provincial differences.
Best for: Families who value structure and contact, and who are comfortable being hands‑on.
United States (established, expensive)
What works: Longstanding legal frameworks, extensive clinic/donor choice, precedent‑rich courts.
Trade‑offs: Extremely high total cost (programme + legal + insurance); state variation; insurance complexity.
Best for: Families with higher budgets seeking an English‑speaking option with broad choice.
Argentina (relationship‑forward; administrative variability)
What works: Strong medical care; counselling culture; intended parents typically named on birth certificate via local practice; relationship‑centric approach.
Trade‑offs: Spanish language; variable timeframes for civil registry processes depending on local policy and court direction; longer average stays when registries slow. Argentina’s processes vary. At the time of writing this, the Intended Parents I’m working with in Argentina are all exiting in good time, however in 2024 there was a period where parents were stuck for months. Like anywhere, the processes must be followed but in Argentina, if processes are not done properly, it can become a bureaucratic nightmare. At the time of writing we are supporting parents on journeys there and don’t see any problems but recommend other destinations over Argentina because of the risk of having to stay longer. Having said that, due to my connections in Argentina, if we ever were to have a third, it’d be in Argentina.
Best for: Families who prioritise ethics and connection and can embrace cultural difference and longer stays when needed.
Mexico (state‑by‑state; proceed only with precise legal mapping)
What works: Rapidly expanding clinic capacity; specific states (e.g., Sinaloa) have clearer pathways; Spanish/English coordination available. Extensive egg donor lists. Established surrogacy industry.
Trade‑offs: Federal framework is incomplete; state‑level variability; enforcement and documentation can be inconsistent; must verify parentage steps by state.
Best for: Families with high tolerance for legal complexity who engage top‑tier legal teams in‑state.
Colombia (court‑driven framework; distinct from Mexico)
What works: Constitutional Court jurisprudence supports gestational surrogacy; growing programme experience; Spanish/English coordination; clearer parentage via court orders.
Trade‑offs: No single statute; processes can require tailored court steps; documentation timelines can vary regionally. Since 2025, only the Intended Father and Surrogate mother can be listed on the birth certificate. The baby’s surname will be automatically given to include both names. There’s a court process Local egg donors, if used, are anonymous and photos cannot be legally shared.
Best for: Families who want Latin America with court‑anchored parentage and are comfortable with judicial filings.
Georgia (status changed/uncertain for foreigners)
What works (historically): Clear legislative framework recognising intended parents from birth; comparatively moderate costs.
Trade‑offs: Only for heterosexual married couples.
Best for: Domestic (Georgian) intended parents; foreigners should treat as restricted unless advised otherwise by current legal counsel.
Ukraine (legal pathway exists; war‑zone reality)
What works: Clear commercial surrogacy framework; experienced clinics.
Trade‑offs: Active war; safety, logistics and insurance considerations; evolving guidance.
Best for: Only those with robust risk tolerance and specialist legal/logistical support. Personally I wouldn’t be risking this at all.
Greece (court‑based altruistic model; recent scandals and policy shifts)
What works: Court pre‑approval model historically available; European location; English widely spoken.
Trade‑offs: High‑profile clinic raids/trafficking allegations and policy tightening; evolving eligibility rules for foreigners and for some family types.
Best for: Only with granular, case‑specific legal advice before any commitment.
South Africa (resident‑centred altruistic model)
What works: Strong court‑approved altruistic framework; excellent medical care; English speaking.
Trade‑offs: Typically requires residency/citizenship; not a straightforward route for foreign non‑residents.
Best for: South African residents or those able to meet residency/legal thresholds.
United Kingdom, Australia & New Zealand (altruistic, post‑birth parental orders)
What works: Clear altruistic frameworks; English speaking; supportive counselling cultures.
Trade‑offs: Parental orders granted post‑birth; advertising/matching restrictions; timelines; primarily for residents.
Best for: Residents planning domestic altruistic journeys.
Israel (resident‑centred; expanded eligibility)
What works: Highly regulated medical system; incremental widening of eligibility in recent years.
Trade‑offs: Primarily for Israeli residents/citizens; complex eligibility and approvals.
Best for: Residents able to navigate local approvals.
Portugal and other Europe (case‑by‑case)
Several European countries permit narrow forms of altruistic surrogacy, often for residents only and with tight medical indications. Foreigners rarely qualify; offerings marketed to foreigners should raise questions. Always seek primary legal sources.
How to decide (my filters)
Ethics first: surrogate’s independent legal advice and counselling, explicit welcome for contact, transparent fees.
Legal map: birth certificate process, court steps, typical post‑birth stay, translation needs.
Risk posture: early‑birth plans, admin slowdowns, policy shifts; who escalates and how.
Fit: language, culture, travel, budget.
References: speak with parents from the last 6–12 months in the same city/state you plan to use.

Starting out — knowing if you are ready

Domestic surrogacy or overseas — how I decided (with every messy detail)
Selecting an agency or program — every question I wish I’d asked

Choosing a country if going overseas — deep dive, no gloss
Egg donor selection — the real criteria, by country and by conscience (long form)
Choosing an egg donor ethically — country rules, questions and long‑term thinking
Beyond looks: kindness, consent and the child’s future questions. Detailed notes for Australia, Canada, Argentina, Colombia and Mexico — with how I chose.
An egg donor is not a checklist. She is a person whose generosity will sit inside your family for life. Here is how I chose and how I now guide others.
What mattered to me
• Character before characteristics: kindness, curiosity, a coherent reason for donating.
• Health and genetics: comprehensive screening and carrier matching with me.
• Story for the future child: what she would say, one day, about why she donated.
• Communication style: comfort with updates now or later, and clarity on contact boundaries.
Country rules and realities (selected)
Australia: Mostly known donation via personal networks or community pages (e.g., Egg Donation Australia). Identity release is standard. Advertising/payment restrictions apply; reimburse expenses only. Expect counselling.
Canada: Culture of known/altruistic donation with strong consent processes; agencies facilitate introductions; identity release common.
Argentina: Donor profiles viewed in clinic; typically you may view photos but cannot retain identifying images; legal landscape evolving.
Colombia: Court‑shaped framework; local donor faces often not shown publicly; clinics manage identity protections; parental rights anchored through court steps.
Mexico: Rules vary by state; confirm if and how donor identity is handled and what may be retained in files; align with state law and clinic policy.
Practical steps I recommend
Start with genetic matching, then values.
Write a plain‑English donor agreement alongside clinic consents, covering future

Starting out — knowing if you are ready

Domestic surrogacy or overseas — how I decided (with every messy detail)
Selecting an agency or program — every question I wish I’d asked

Choosing a country if going overseas — deep dive, no gloss
Choosing your surrogate and building the relationship
How to choose a surrogate and nurture the relationship
Practical advice on matching with a surrogate, from Australian friendships to close bonds in Canada and Argentina. Why more contact often means a better journey.
I wanted a surrogate I would be friends with outside the surrogacy context. That is how both of my journeys worked best. Your preference may differ, but here is what I learned.
Australia taught me patience
There are no agencies or formal matching services here. You meet in community groups. You chat. You visit. You cook meals together. It feels like dating because it is. You are building trust. We did all that and more. We had a positive. Then a loss. The friendship is still strong and that matters.
Canada and Argentina showed me structure with heart
In Canada we built a fast friendship because she had already been a surrogate. We spoke every couple of hours during the pregnancy. In Argentina language differences became a source of laughs. We texted through a translator and shared playlists for the baby. We were supported by coordinators who valued counselling and contact.
Contact preferences differ
Some intended parents want minimal contact. Some surrogates prefer that. Many people want something in the middle or very connected. I suggest leaning towards more contact if both parties are comfortable. Share scans, messages, the ordinary details of a week. Those threads become the fabric of a shared story your child will one day hear.
Questions to discuss early
How often will we chat. How will decisions be made. What are expectations about birth and hospital time. What will contact look like after birth. What happens if plans change. Put it in writing with independent legal advice for everyone. Then be human and flexible as life unfolds.
Closing thought
A strong relationship does not remove all bumps. It does give you a way to travel over them together. The best journeys I have seen are respectful, warm and clear from day one.

Starting out — knowing if you are ready

Domestic surrogacy or overseas — how I decided (with every messy detail)
Selecting an agency or program — every question I wish I’d asked

Choosing a country if going overseas — deep dive, no gloss
Managing pregnancy and stress from far away
Managing a surrogacy pregnancy from overseas
How to stay connected and calm when you live far from your surrogate. Update rhythms, agency roles, travel plans and the practicalities that reduce stress.
Pregnancy is a season of waiting. Distance makes the quiet moments louder. Here is what helped us and the families I support.
Set an update rhythm
Agree the channels and frequency. We used WhatsApp and set expectations around appointments, test results and casual check ins. A small message after a scan goes a long way. If you work with a program, ask who posts updates and when. Clarity reduces worry.
Share the ordinary
Playlists for the baby. Photos of the nursery. School updates from older siblings. These little exchanges build connection that money cannot buy. They also make the big moments feel less overwhelming because you are already in steady contact.
Plan travel with buffers
Babies do not read calendars. Frida arrived four weeks early while I was in a hardware store buying a toilet seat for a rushed renovation. If flying in for the birth, arrive early. Book flexible tickets and accommodation near the hospital. Have someone on standby to care for children at home.
Prepare a hospital plan
Confirm who is allowed in the room, language support, skin to skin preferences and newborn feeding choices. Ask the hospital what documents they need from you. Have translations ready if required. Pack copies of key forms in both paper and digital folders.
Look after yourself
Eat, sleep and keep perspective. This is an exercise in shared trust. Counselling helps. So does a walk outside and a laugh on a hard day. Your surrogate is carrying the physical load. Carry the emotional load together.
Closing thought
Distance is real. So is connection. With clear plans and gentle routines, you can feel close even when you are far away.

Starting out — knowing if you are ready

Domestic surrogacy or overseas — how I decided (with every messy detail)
Selecting an agency or program — every question I wish I’d asked

Choosing a country if going overseas — deep dive, no gloss
Birth and the first weeks — two stories and many lessons
Surrogacy birth stories. Missing one birth and making the most of the first weeks
What the birth felt like across two countries, what I did right, what I would change, and how to settle in with a newborn in a foreign city.
My two birth stories could not be more different. In Canada I arrived days before and held my son within minutes. In Argentina I arrived four and a half days after my daughter was born and said my first hello with a mix of joy and regret. Both experiences taught me what matters most.
When you miss the birth
If baby comes early and you are not there, breathe. You have not failed. You are still the parent. Focus on arriving safely and being present the moment you walk in. Ask for as many photos and video calls as everyone is comfortable with. When you meet your baby, take the time you need for skin to skin and quiet.
When you are there on time
Hospitals have their own rhythms. Clarify who can be in the room and how you will share time respectfully. Check feeding plans and paperwork. Thank staff. Thank your surrogate. Do not rush the first cuddle. There is a before and an after. Let yourself feel both.
The first weeks in a foreign city
Keep it simple. Choose accommodation close to where you’ll need to be. Learn the basic words you need. Use a baby carrier. Accept help from coordinators and new friends. I took slow walks, did paperwork during naps, and kept meals easy. When my mum and my son arrived, we added small adventures like a day trip to Mendoza between appointments. Make the most of your new city, it’ll be your home for the next few months.
Admin without losing your mind
Create a single digital folder with passports, birth certificates, medical letters and translations. Keep paper copies in a zip folder. Label everything. Each time someone asks for a document, save the request inside the folder with a date so you can track what was provided.
Closing thought
Whether you greet your baby two minutes or four days after birth, the same truth holds. You are here. You are ready. You will find a rhythm. The city turns into a memory you will tell for the rest of your life.

Starting out — knowing if you are ready

Domestic surrogacy or overseas — how I decided (with every messy detail)
Selecting an agency or program — every question I wish I’d asked

Choosing a country if going overseas — deep dive, no gloss